Scleroderma
😏cidpusa.orgSearch Cidpusa web
learn Scleroderma
What Causes Scleroderma?
Scleroderma, is a autoimmune disease and is triggered by Mycoplasma. Studies of twins suggest it is also not inherited.
Abnormal immune or inflammatory activity: Like many other rheumatic disorders, scleroderma is believed to be an autoimmune disease. An autoimmune disease is one in which the immune system, for unknown reasons, turns against one's own body.
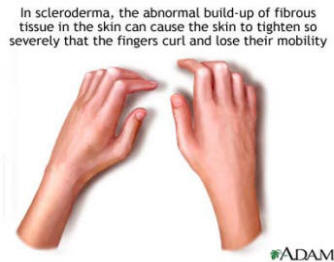
In scleroderma, the immune system is thought to stimulate cells called fibroblasts so they produce too much collagen. The collagen forms thick connective tissue that builds up within the skin and internal organs and can interfere with their functioning. Blood vessels and joints can also be affected.
Genetic makeup: While genes seem to put certain people at risk for scleroderma and play a role in its course, the disease is not passed from parent to child like some genetic diseases.
Environmental triggers: Research suggests that exposure to some environmental factors may trigger sclerodermalike disease (which is not actually scleroderma) in people who are genetically predisposed to it. Suspected triggers include mycoplasma infection, viral infections, certain adhesive and coating materials, and organic solvents such as vinyl chloride or trichloroethylene. But no environmental agent has been shown to cause scleroderma. In the past, some people believed that silicone breast implants might have been a factor in developing connective tissue diseases such as scleroderma. But several studies have not shown evidence of a connection.
Hormones: By the middle to late childbearing years (ages 30 to 55) women develop scleroderma 7 to 12 times more often than men. Because of female predominance at this and all ages, scientists suspect that hormonal differences between women and men play a part in the disease. However, the role of estrogen or other female hormones has not been proven.
Who Gets Scleroderma?
A lthough scleroderma is more common in women, the disease also occurs in men and children. It affects people of all races and ethnic groups. However, there are some patterns by disease type. For example:
- Localized forms of scleroderma are more common in people of European descent than in African Americans. Morphea usually appears between the ages of 20 and 40, and linear scleroderma usually occurs in children or teenagers.
- Systemic scleroderma, whether limited or diffuse, typically occurs in people from 30 to 50 years old. It affects more women of African American than European descent.
Because scleroderma can be hard to diagnose and it overlaps with or resembles other diseases, scientists can only estimate how many cases there actually are. Estimates for the number of people in the United States with systemic sclerosis range from 40,000 to 165,000. By contrast, a survey that included all scleroderma-related disorders, including Raynaud's phenomenon, suggested a number between 250,000 and 992,500.
For some people, scleroderma (particularly the localized forms) is fairly mild and resolves with time. But for others, living with the disease and its effects day to day has a significant impact on their quality of life.
How Is Scleroderma Diagnosed?
Depending on your particular symptoms, a diagnosis of scleroderma may be made by a general internist, a dermatologist (a doctor who specializes in treating diseases of the skin, hair, and nails), an orthopaedist (a doctor who treats bone and joint disorders), a pulmonologist (lung specialist), or a rheumatologist (a doctor specializing in treatment of musculoskeletal disorders and rheumatic diseases). A diagnosis of scleroderma is based largely on the medical history and findings from the physical exam. To make a diagnosis, your doctor will ask you a lot of questions about what has happened to you over time and about any symptoms you may be experiencing. Are you having a problem with heartburn or swallowing? Are you often tired or achy? Do your hands turn white in response to anxiety or cold temperatures?
Once your doctor has taken a thorough medical history, he or she will perform a physical exam. Finding one or more of the following factors can help the doctor diagnose a certain form of scleroderma:
- changed skin appearance and texture, including swollen fingers and hands and tight skin around the hands, face, mouth, or elsewhere
- calcium deposits developing under the skin
- changes in the tiny blood vessels (capillaries) at the base of the fingernails
- thickened skin patches.
- Continue to next page for treatment of scleroderma