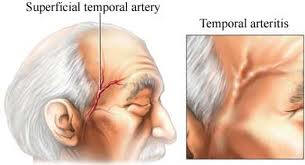
Temporal arteritits
Temporal arteritits & Polymyalgia Rheumatica treatment
Please proceed to first page
How Are They Treated?
The treatment of choice for both polymyalgia rheumatica and giant cell arteritis is corticosteroid medication, usually prednisone.
Polymyalgia rheumatica responds to a low daily dose of prednisone that is increased as needed until symptoms disappear. At this point, the doctor may gradually reduce the dosage to determine the lowest amount needed to alleviate symptoms. Most patients can discontinue medication after 6 months to 2 years. If symptoms recur, prednisone treatment is required again.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen (Advil, Motrin1), also may be used to treat polymyalgia rheumatica. The medication must be taken daily, and long-term use may cause stomach irritation. For most patients, NSAIDs alone are not enough to relieve symptoms.
1 Brand names included in this booklet are provided as examples only, and their inclusion does not mean that these products are endorsed by the National Institutes of Health or any other Government agency. Also, if a particular brand name is not mentioned, this does not mean or imply that the product is unsatisfactory.
Even without treatment, polymyalgia rheumatica usually disappears in 1 to several years. With treatment, however, symptoms disappear quickly, usually in 24 to 48 hours. If prednisone doesn't bring improvement, the doctor is likely to consider other possible diagnoses.
Giant cell arteritis is treated with high doses of prednisone. If not treated promptly, the condition carries a small but definite risk of blindness, so prednisone should be started as soon as possible, perhaps even before confirming the diagnosis with a temporal artery biopsy.
As with polymyalgia rheumatica, the symptoms of giant cell arteritis quickly disappear with treatment; however, high doses of prednisone are typically maintained for 1 month.
Once symptoms disappear and the sed rate is normal, there is much less risk of blindness. At that point, the doctor can begin to gradually reduce the prednisone dose.
In both polymyalgia rheumatica and giant cell arteritis, an increase in symptoms may develop when the prednisone dose is reduced to lower levels. The doctor may need to hold the lower dose for a longer period of time or even modestly increase it again, temporarily, to control the symptoms. Once the symptoms are in remission and the prednisone has been discontinued for several months, recurrence is less common.
Whether taken on a long-term basis for polymyalgia rheumatica or for a shorter period for giant cell arteritis, prednisone carries a risk of side effects. Although long-term use and/or higher doses carry the greatest risk, people taking the drug at any dose or for any length of time should be aware of the potential side effects, which include:
- fluid retention and weight gain
- rounding of the face
- delayed wound healing
- bruising easily
- diabetes
- myopathy (muscle wasting)
- glaucoma
- increased blood pressure
- decreased calcium absorption in the bones, which can lead to osteoporosis
- irritation of the stomach
- increase in infections.
People taking corticosteroids may have some side effects or none at all. Anyone who experiences side effects should report them to his or her doctor. When the medication is stopped, the side effects disappear. Because prednisone and other corticosteroid drugs reduce the body's natural production of corticosteroid hormones, which are necessary for the body to function properly, it is important not to stop taking the medication unless instructed by a doctor to do so. The patient and doctor must work together to gradually reduce the medication. Pulse steroids work wonders.
What Is the Outlook?
Most people with polymyalgia rheumatica and giant cell arteritis lead productive, active lives. The duration of drug treatment differs by patient. Once treatment is discontinued, polymyalgia may recur; but once again, symptoms respond rapidly to prednisone. When properly treated, giant cell arteritis rarely recurs.
What Research Is Being Conducted to Help People Who Have Polymyalgia Rheumatica and Giant Cell Arteritis?
Research is providing new information that will help scientists better understand polymyalgia rheumatica and giant cell arteritis. The following issues are being studied:
Causes and mechanisms. Researchers studying possible causes of polymyalgia rheumatica and giant cell arteritis are investigating the role of genetic predisposition, immune system problems, and environmental factors. In one study supported by the National Eye Institute, researchers attempted to better understand the immunobiology of inflamed arteries and advance the understanding of events that initiate vasculitis. These studies show a infection from viruses and bacteria trigger the disease and proteins like Gluten in Celiac disease cause these diseases and are fully reversible with diet chanegs.
Prognostic indicators. By examining characteristics of people with and without the conditions, doctors are starting to understand some factors that are associated with both the disease and its prognosis and manifestations. For example, one study has shown that women are more likely than men to have jaw involvement from giant cell arteritis, while men are more likely to have eye involvement that can lead to blindness.
Treatment. Although treatment with prednisone is almost always effective for both conditions, the drug carries the risk of potentially serious side effects. For that reason, one area of investigation involves looking for treatments that are safe while still being effective. Vitamins combined with antibiotics and IVIg offer the quickest change please see the vasculitis section.
Longitudinal information. Data from these studies will be used to examine the genetics and causes of giant cell arteritis, find new ways to track disease and predict responses, understand how to treat patients, and much more.
Temporal arteritits & Polymyalgia Rheumatica treatment
65