"It's very common for neuropathies to affect neurons with the longer axons, for example those that innervate the legs and feet," says Popko. It has been previously suggested that hereditary sensory neuropathy might be connected with disabled trafficking along the axons. There have been mutations found in two genes that form a complex essential for survival of sensory neurons, and this complex is thought to be transported along the neurons by dynein.
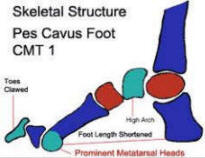
Charcot Marie Tooth
If CMT is suspected, the physician may order electrodiagnostic tests for the patient. This testing consists of two parts: nerve conduction studies and electromyography (EMG). During nerve conduction studies, electrodes are placed on the skin over a peripheral motor or sensory nerve. These electrodes produce a small electric shock that may cause mild discomfort. This electrical impulse stimulates sensory and motor nerves and provides quantifiable information that the doctor can use to arrive at a diagnosis. EMG involves inserting a needle electrode through the skin to measure the bioelectrical activity of muscles. Specific abnormalities in the readings signify axon degeneration. EMG may be useful in further characterizing the distribution and severity of peripheral nerve involvement.
If all other tests seem to suggest that a patient has CMT, a neurologist may perform a nerve biopsy to confirm the diagnosis. A nerve biopsy involves removing a small piece of peripheral nerve through an incision in the skin. This is most often done by removing a piece of the nerve that runs down the calf of the leg. The nerve is then examined under a microscope. Patients with CMT1 typically show signs of abnormal myelination. Specifically, "onion bulb" formations may be seen which represent axons surrounded by layers of demyelinating and remyelinating Schwann cells. Patients with CMT2 usually show signs of axon degeneration.
Genetic testing is available for some types of CMT and may soon be available for other types; such testing can be used to confirm a diagnosis. In addition, genetic counseling is available to parents who fear that they may pass mutant genes to their children.